THE WHO CONTRIBUTES TO NPHL
by
Moses Nyambalo Phiri in collaboration with Happy Abraham Manda, Mr. Henry Limula and Settie Kanyanda.
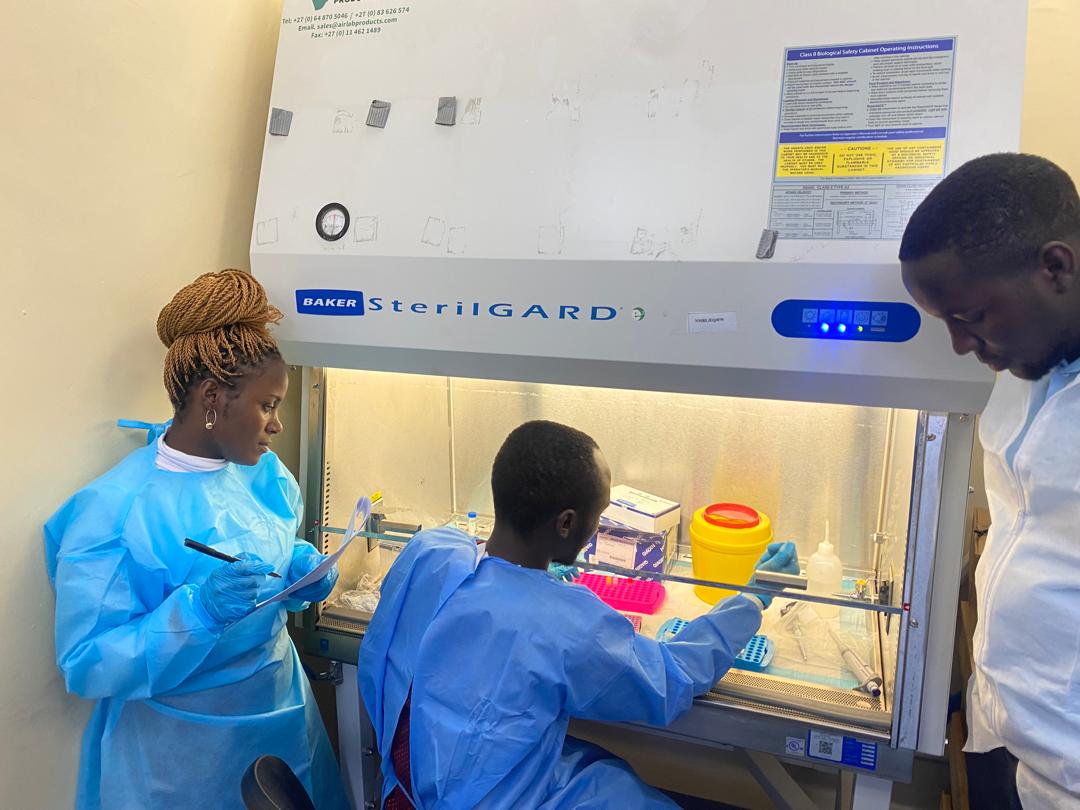
The World Health Organisation (WHO), with support from UK Aid (UKAID), has made a significant donation delivery of essential laboratory items to the National Public Health Laboratories (NPHL) to the National Public Health Laboratory, PHIM. This timely contribution will aid Malawi’s capacity to monitor and respond to various public health threats, including the ongoing Mpox outbreak
The NPHRL plays a pivotal role in Malawi’s health surveillance systems, tracking a range of diseases. Currently, a key focus is the surveillance of Mpox, a viral disease that has affected several African nations, with Malawi reporting six confirmed cases by May 15th, 2025.

To ensure the safety of frontline health workers during critical activities such as outbreak investigations, sample collection, and the implementation of control measures, the WHO generously donated Personal Protective Equipment (PPEs). The consignment included vital items such as gloves, aprons, and gumboots.

Receiving the donations on behalf of the NPHRL, Mr. Joseph Bitilinyu Bangoh expressed his sincere appreciation to the WHO for their prompt response citing the current response activities NPHL – PHIM is undertaking to contain Mpox. He further acknowledged the WHO’s consistent support to PHIM during the Mpox pandemic and in the surveillance of other significant diseases, including conjunctivitis, cholera, and influenza.
He earnestly appealed to the WHO to maintain their invaluable assistance, even in the face of potential financial constraints affecting international organizations. Dr. Nelly Yatich, representing the WHO during the donation, warmly assured the PHIM staff of the WHO’s unwavering commitment to supporting Malawi, particularly during health crises like the current Mpox outbreaks. She emphasized the WHO’s proactive approach in providing the necessary equipment swiftly to aid in the effective management of Mpox cases.

During the event, Mr. Bangoh also formally welcomed Mr. Ishmael Bashir, a resident delegated from the (WHO) to work at PHIM, NPHRL. He reiterated his gratitude to the WHO for this additional support, highlighting that Mr. Bashir’s presence will provide valuable insight into Malawi’s needs and facilitate targeted assistance.
This has indicated the robust collaboration that exists between the World Health Organisation (WHO) and the Public Health Institute of Malawi (PHIM). Their joint efforts are crucial for enhancing Malawi’s public health systems and protecting its citizens. This partnership is expected to continue with future collaborations.
Special Thanks to: