Malawi’s Latest Health Bulletin Confirms 14 New Mpox Cases
Weekly IDSR Report Highlights Ongoing Public Health Surveillance
A new report from the Public Health Institute of Malawi (PHIM) provides a detailed look into the country’s public health landscape, with a significant focus on the ongoing Mpox outbreak. The latest Integrated Disease Surveillance and Response (IDSR) bulletin for Epidemiological Week 37 (September 8-14, 2025) confirms an additional 14 new Mpox cases, bringing the cumulative total to 110.
Public Health Events in Epi-week 37
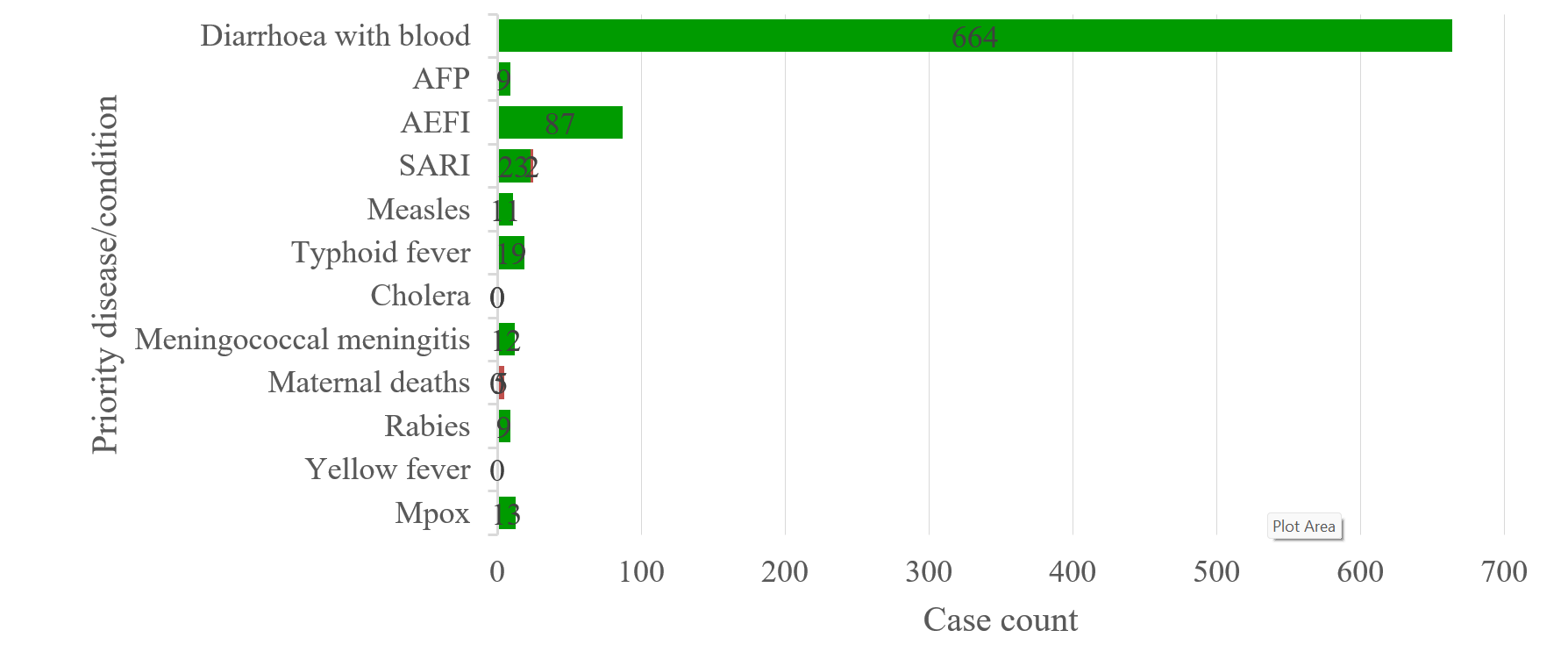
Notifiable diseases/conditions alerts reported in Epi-week 37 in Malawi (Data accessed on 17 September 2025)
Outbreak at a Glance
According to the report, the outbreak continues to be actively monitored, with key metrics updated for the latest week. As of September 14, 2025, the breakdown of cases is as follows:
- Total Confirmed Cases: 110 laboratory-confirmed cases in Malawi, plus 2 cross-border cases.
- New Cases: 13 new cases were recorded during Epidemiological Week 37.
- Patient Status: 84 individuals have been discharged, 23 are currently in isolation, and 2 are lost to follow-up.
- Deaths: One death has been confirmed since the start of the outbreak, with no new deaths reported in Week 37.
- Contact Tracing: A total of 1,167 contacts have been identified and are being monitored.
Affected Districts and Demographics
The age range of confirmed cases spans from 2 to 75 years. The outbreak has now been reported in 12 districts across the country, highlighting its widespread nature. The districts include Lilongwe, Mangochi, Ntcheu, Salima, Likoma, Nkhatabay, Blantyre, Mzimba South, Ntchisi, Karonga, Zomba, and Chitipa.
Public Health Surveillance and Response
The Public Health Institute of Malawi (PHIM) is mandated to protect public health through robust surveillance, early warning, and outbreak containment. The IDSR system’s overall reporting stood at an impressive 90.7% for completeness and 83.3% for timeliness on the One Health Surveillance Platform (OHSP) during this reporting period.
In response to the Mpox outbreak and other public health events, a comprehensive multi-sectoral approach has been implemented. Key measures include:
- Incident Management System (IMS): The IMS has been activated to coordinate all response efforts.
- Rapid Response Teams: Functional Rapid Response Teams (DRRTs) have been deployed at both national and district levels. These teams are actively engaged in collecting blister swab samples, conducting contact tracing, and following up on cases.
- Multi-sectoral Collaboration: A “One Health” approach is being utilized, involving the collaboration of both human and animal health workers at national and district levels to enhance disease surveillance.
- Training and Capacity Building: PHIM has been training the National Emergency Medical Team, surge teams, and frontline health workers to ensure a skilled and ready response force.
- Risk Communication: The Ministry of Health is actively engaged in risk communication and community engagement activities to educate the public on disease prevention and containment.
In addition to Mpox, the surveillance system also detected other public health events in Epidemiological Week 37:
- Severe Acute Respiratory Infections (SARI): 42 cases, 3 deaths
- Diarrhoea with blood: 718 cases
- Adverse Events Following Immunization (AEFI): 83 cases
- Typhoid fever: 23 cases
- Acute flaccid paralysis (AFP): 6 cases
- Maternal Deaths: 5 deaths
- Meningococcal meningitis: 4 cases, 1 death
Looking Forward
The report concludes with specific recommendations for improving the public health response. These include enhancing reporting timeliness and signal detection, conducting prompt risk assessments for all verified events, and strengthening routine immunization programs.