1. Coordination & Leadership
The national coordination mechanism is led by the Public Health Institute of Malawi (PHIM) through the activated Public Health Emergency Operations Centre (PHEOC). This leadership structure ensures that all technical sub-committees are synchronized in their response to the 682 cumulative suspected cases recorded as of February 08, 2026. Daily briefing sessions facilitate rapid resource mobilization and deployment to active hotspots like Blantyre and Zomba, ensuring that district-level task forces have the administrative support required to implement local interventions.
Furthermore, the leadership is focused on harmonizing the efforts of international partners, NGOs, and government line ministries to avoid duplication of work. Strategic meetings are currently prioritizing the containment of the 8 new cases identified in the last 24 hours across Blantyre, Zomba, Mwanza, and Chikwawa. By maintaining a high level of political commitment and multi-sectoral involvement, the coordination pillar serves as the backbone of the entire cholera elimination strategy during this critical Epidemiological Week 6.
2. Surveillance & Laboratory
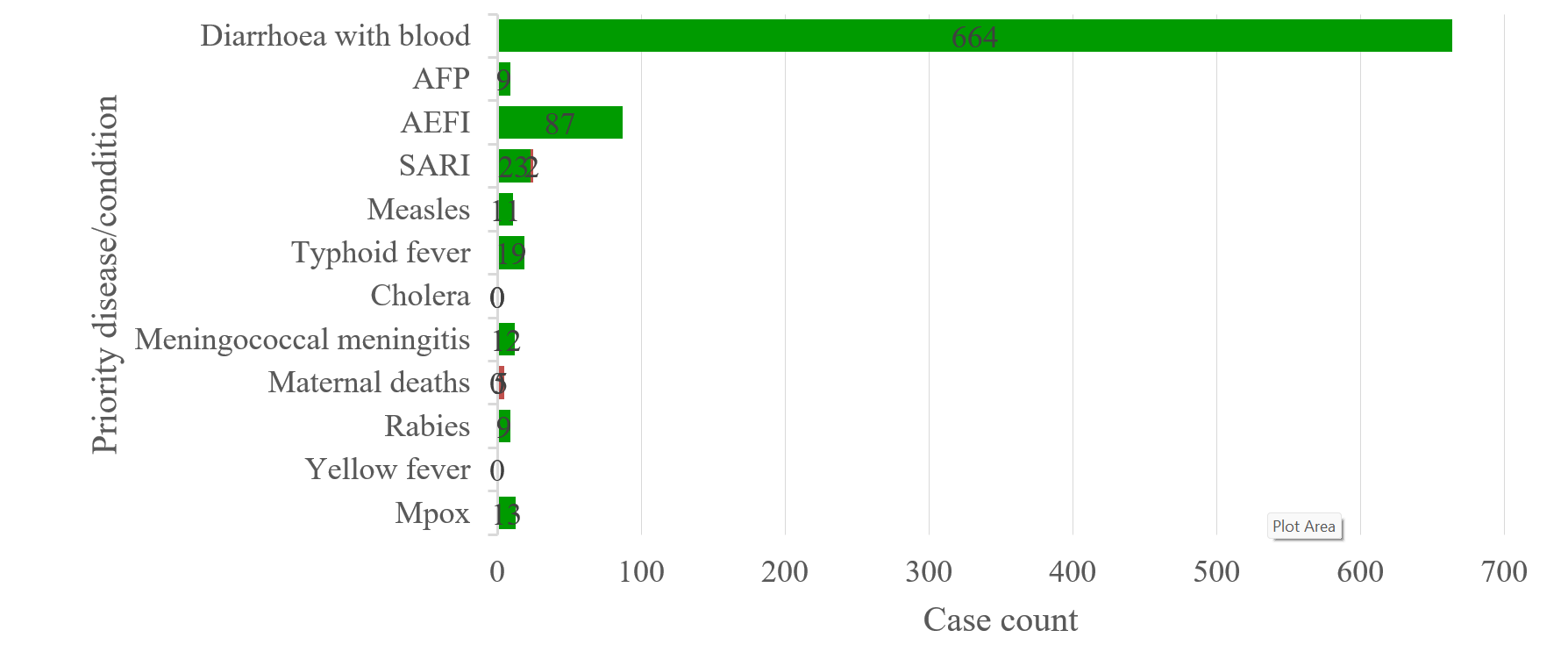
Surveillance teams are employing enhanced Case-Area Targeted Interventions (CATI) to track the progression of the outbreak, which has now touched 28 districts cumulatively. The laboratory component is essential for validating the 77 local confirmed cases and managing the diagnostic backlog of the 682 suspected cases currently in the system. High-frequency RDT testing is being conducted in the 6 currently active districts, providing the granular data needed to identify specific Traditional Authorities (TAs) where Vibrio cholerae is circulating most aggressively.
To further strengthen laboratory capacity, PHIM is distributing additional RDT kits and culture media to regional laboratories in the Southern and Central regions. This effort is aimed at reducing the turn-around time for culture confirmation, which is vital for monitoring antibiotic sensitivity and strain variations. The integration of community-level surveillance with facility data allows for a more comprehensive understanding of the 2.59% Case Fatality Rate, highlighting whether deaths are occurring due to late detection or clinical management gaps.
3. Case Management
Case management protocols have been standardized across all 6 active CTUs to ensure that patients receive high-quality rehydration and antibiotic therapy. As of today, 5 patients remain admitted, while 77 have been successfully discharged, reflecting a high recovery rate for those who seek care early. Technical supervisors are conducting bedside mentoring for clinical staff in Blantyre and Zomba to ensure strict adherence to the WHO-recommended dehydration assessment and treatment algorithms, which are crucial for maintaining the declining CFR trend.
The case management pillar is also focusing on the establishment of more Community Oral Rehydration Points (ORPs) to provide immediate intervention for patients in remote areas. This “early rehydration” strategy is designed to stabilize patients before they are transported to CTUs, thereby preventing severe complications and deaths in transit. Ongoing audits of the 2 verified deaths are being used to identify specific clinical areas that require reinforcement, such as the management of pediatric cases and patients with underlying comorbidities.
4. Water, Sanitation & Hygiene (WASH)
The WASH pillar is aggressively targeting the environmental drivers of cholera by chlorinating over 150 water points in the hotspots of Blantyre and Chiradzulu. Environmental health officers are conducting “pot-to-pot” chlorination and distributing Water Guard to households located within a 100-meter radius of any new case reported in the last 24 hours. These efforts are aimed at breaking the transmission cycle in high-density urban areas where sanitation infrastructure is under significant pressure from the ongoing rainy season.
In addition to water treatment, the WASH teams are promoting the construction and maintenance of emergency pit latrines in CTUs and transit sites. Handwashing stations with soap or 0.05% chlorine solution have been deployed at markets and bus depots in the 6 active districts. By integrating water quality monitoring with sanitation improvements, the WASH pillar addresses both the source and the spread of the pathogen, which is fundamental to achieving a sustainable reduction in the 682 cumulative suspected cases.
5. Infection Prevention & Control (IPC)
IPC measures have been intensified within all health facilities to prevent nosocomial transmission among healthcare workers and other patients. Strict zoning of CTUs—separating triage, treatment, and recovery areas—is being monitored through daily checklists and supervisory visits. The provision of Personal Protective Equipment (PPE) and high-strength chlorine for surface disinfection is prioritized for facilities reporting the 8 new cases in the current reporting period, ensuring that the hospital environment does not become a secondary source of infection.
Beyond the health facility, IPC teams are also conducting terminal disinfection of the homes of the 682 suspected cases. This household-level intervention includes the spraying of latrines and living areas with 2% chlorine solution and the safe disposal of contaminated materials. Training for community volunteers in basic IPC practices ensures that localized cleaning can begin immediately after a case is suspected, significantly reducing the risk of household clusters and intra-familial spread.
6. Risk Communication & Community Engagement (RCCE)
The RCCE pillar is utilizing a variety of channels, including community radio, mobile vans, and house-to-house visits, to disseminate life-saving information. Current messaging focuses on the importance of early care-seeking and the correct preparation of Oral Rehydration Salts (ORS) at home. Feedback from community dialogues indicates that while awareness of cholera is high, there are still myths regarding the causes of the disease that need to be addressed through targeted engagement with traditional and religious leaders in the 28 affected districts.
Engagement strategies are also being tailored to reach the male demographic, which currently represents 58% of confirmed cases. Targeted interventions at “drinking joints,” markets, and transport hubs in Blantyre and Lilongwe are being conducted to promote hygiene among high-risk groups. By empowering communities to take ownership of the response, the RCCE pillar facilitates the adoption of preventive behaviors that are essential for bringing the Case Fatality Rate down toward the WHO target of less than 1%.
7. Logistics & Supply Chain
The logistics sub-committee is managing the critical flow of supplies, including IV fluids, RDT kits, and cholera treatment beds, to the most burdened districts. Real-time inventory tracking at the national warehouse ensures that stocks are replenished before they reach a critical low, particularly in the Southern region hotspots. The current pipeline is healthy, with enough supplies to manage the expected surge during the peak of the rainy season, but specialized logistics for the distribution of cold-chain OCV are also being finalized.
Logistics teams are also responsible for the maintenance of ambulances and utility vehicles used for case transport and surveillance. In districts like Mwanza and Chikwawa, where terrain can be difficult, the deployment of 4×4 vehicles is prioritized to ensure that surveillance teams can reach remote Traditional Authorities. This logistical support is the “engine” of the response, allowing for the timely delivery of interventions to the 8 new suspected cases identified in the last 24 hours.
8. Oral Cholera Vaccine (OCV)
The OCV pillar is currently in the advanced stages of planning for a reactive vaccination campaign in the highest-burden areas of Blantyre and Zomba. Micro-plans have been developed to target over 500,000 individuals in the most affected Traditional Authorities, where the density of the 682 suspected cases is highest. The Ministry of Health is coordinating with the International Coordinating Group (ICG) to secure the necessary doses, emphasizing the vaccine’s role as a powerful tool to supplement WASH and clinical management interventions.
Preparation for the OCV campaign includes training for vaccinators and the deployment of cold-chain equipment to the district level. Community mobilization teams are already on the ground in Blantyre, sensitizing the public about the vaccine to ensure high uptake once the doses arrive. This strategic use of OCV is intended to create a “firebreak” of immunity in urban hotspots, preventing the outbreak from evolving into a massive national surge as seen in previous years.
9. Border Health & Points of Entry (PoE)
Border health surveillance is a critical priority, given that 41 of the total confirmed cases are imported. Screening stations at Mwanza, Dedza, and Songwe have been reinforced with additional health personnel and RDT kits to detect and isolate suspected cases entering the country. Collaboration with neighboring countries’ health authorities is ongoing to share epidemiological data and synchronize cross-border interventions, particularly for mobile populations like truck drivers and traders.
In addition to screening, hygiene facilities at major border crossings are being upgraded to provide travelers with safe water and handwashing options. The identification of imported cases allows Malawi to manage the “seeding” of the outbreak from outside its borders, protecting the 22 districts that are currently not reporting active cases. This pillar remains highly vigilant as regional travel increases, ensuring that any new imported threat is contained before it reaches the domestic population centers.
10. Data Management & Reporting
The data management pillar ensures the integrity and timeliness of the national situation reports, which are published daily by PHIM. Using digitized reporting tools, data from all 28 affected districts is collated and analyzed to produce the metrics seen in today’s SitRep, such as the 2.59% CFR and the breakdown of suspected cases. This rigorous data handling allows for the identification of trends, such as the rising burden in Chiradzulu, which in turn informs the shifting of resources and technical focus.
Analysts are currently focusing on improving the “line-listing” of all suspected cases to ensure that every patient is tracked from admission to discharge or death. This detailed tracking is essential for calculating accurate epidemiological indicators and for identifying geographic clusters that require immediate CATI intervention. The transition to real-time data entry at the facility level is reducing reporting delays, providing the PHEOC with the “live” intelligence needed to manage the dynamic outbreak.
11. Human Resources for Health
The surge in 682 suspected cases has necessitated the deployment of additional healthcare workers to the most affected districts. The Ministry of Health is redistributing staff from non-active areas and recruiting temporary health workers to staff CTUs and surveillance teams in Blantyre and Zomba. This human resource strategy includes not just clinical staff, but also data clerks, environmental health officers, and community volunteers who form the frontline of the integrated response.
To maintain staff morale and safety, ongoing training in cholera management and IPC is provided, along with the consistent provision of PPE. Psychosocial support for frontline workers is also being integrated into the response, recognizing the intense pressure of managing an active outbreak during the rainy season. By ensuring that the “human engine” of the response is well-supported and trained, the pillar safeguards the quality of care provided to the 5 patients currently admitted and all future suspected cases.
12. Research & Innovation
The research pillar is conducting operational studies to understand the factors driving the 58% male infection rate and the persistence of the outbreak in certain Traditional Authorities. Genomic sequencing of Vibrio cholerae samples is being prioritized to track the evolution of the bacteria and to identify any emerging drug resistance. These scientific insights are fed directly back into the coordination pillar to refine clinical management protocols and community engagement strategies based on local evidence.
Innovation is also being seen in the use of GIS mapping to visualize the 682 suspected cases against water point functionality and sanitation coverage. This spatial analysis helps in predicting future hotspots and in prioritizing WASH interventions for maximum impact. By marrying scientific research with operational response, Malawi is not only reacting to the current outbreak but also building a knowledge base to prevent future epidemics and achieve the long-term goal of cholera elimination.
13. Mental Health & Psychosocial Support (MHPSS)
MHPSS services are being integrated into CTUs to support patients and their families who are coping with the trauma of infection and the stigma often associated with cholera. Counselors are available to provide bereavement support to the families of the 2 verified deaths, helping them to process their loss while also providing education on safe burial practices. This holistic approach ensures that the medical response is complemented by emotional care, which is vital for community trust and cooperation during an outbreak.
Furthermore, MHPSS teams are working with community leaders to combat the stigmatization of the 77 discharged patients and their families. By promoting a supportive environment, the pillar encourages individuals with symptoms to seek care without fear of social exclusion. This social support is a key factor in the early detection of cases and the overall success of the integrated response, as it addresses the psychological barriers to effective public health intervention.
Authored & Published By
Moses Nyambalo Phiri
Public Health Institute of Malawi
Ministry of Health, Republic of Malawi