Epidemiological
Intelligence
Surveillance Update: 20th January, 2026
PUBLISHED BY
Moses Nyambalo Phiri
Executive Case Briefing
On 18th January 2026, the Public Health Institute of Malawi confirmed a new case in Salima District involving an 18-year-old female. This diagnostic confirmation, occurring 12 days after the initial hospital presentation, underscores the vital importance of molecular validation in managing the current outbreak, which has now accumulated 148 confirmed cases.
148
National Total
01
New Salima Case

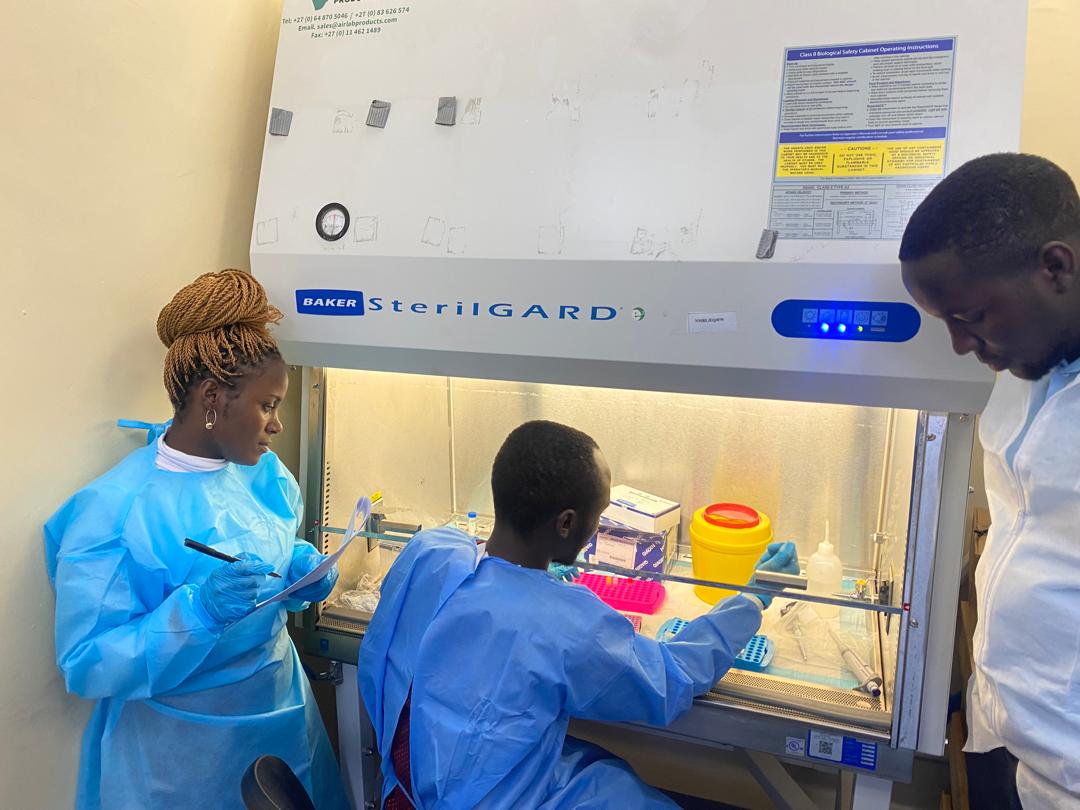
Fig A: Typical clinical presentation observed in recent Central Region cases.
Operational Response & Data Insights
District Sentinel Analysis
The notification from Salima District hospital on January 6th, followed by PCR confirmation on the 18th, highlights a critical window for containment. The Salima District Rapid Response Team (DRRT) has prioritized contact tracing around this 18-year-old female, who represents a significant demographic shift as younger populations increasingly become points of entry for the virus in rural settings.
Operationally, the focus is now on “Ring Surveillance.” By mapping the patient’s interactions within the 21-day incubation period, the DRRT is effectively creating a safety perimeter. This prevents the transition from a sporadic case to a localized cluster, which is essential given Salima’s role as a transit and tourism hub that could easily facilitate cross-district transmission.
One Health Surveillance Matrix
The activation of the Incident Management System (IMS) signifies a transition to high-alert status. This multisectoral One Health approach is critical because it integrates human clinical data with animal health monitoring. Understanding the zoonotic potential of Mpox in Malawi is key to identifying the environmental reservoirs that might be driving these persistent “sporadic” infections across different districts.
Furthermore, the IMS structure allows for real-time resource reallocation. As shown in the surveillance matrix, deployment of functional Rapid Response Teams (RRTs) is not static; it follows the trajectory of new confirmations. The training of National Emergency Medical Teams ensures that the surge capacity is prepared for any sudden spikes in severity or volume that may arise as the virus moves through the lake-shore communities.
Diagnostic Efficiency Trends
Diagnostic integrity is the cornerstone of the Malawi Mpox response. The PCR-based testing of lesion swabs provides the definitive evidence needed to trigger public health interventions. While the turnaround time for the Salima case reflects the logistical challenges of sample transport from district to central labs, the successful confirmation demonstrates a robust end-to-end diagnostic pipeline that can handle highly infectious specimens.
Looking forward, the focus is on reducing the “symptom-to-confirmation” latency. By empowering district-level human and animal health workers through advanced training, PHIM aims to improve early suspicion and immediate sample collection. This diagnostic intelligence ensures that clinical management, including isolation and symptomatic treatment, begins at the earliest possible stage, significantly improving patient outcomes and reducing secondary attack rates.

Containment Strategy: Infrastructure & Resilience
The strategic deployment of dedicated Mpox Isolation Units is a vital component of Malawi’s health system resilience. By physically separating Mpox management from general medical wards, PHIM effectively mitigates the risk of nosocomial transmission. These units are not merely physical structures; they represent a specialized clinical ecosystem equipped with advanced waste management protocols and high-frequency disinfection cycles, ensuring that healthcare workers remain protected while delivering intensive supportive care.
Beyond the immediate benefit of containment, these facilities foster clinical excellence through specialization. Staff assigned to these units are trained in specific lesion care, pain management, and the identification of secondary bacterial infections. This concentrated expertise is particularly crucial for younger patients, such as the 18-year-old from Salima, ensuring they receive evidence-based care in a dignifying and safe environment that prioritizes both physical recovery and community protection.
Macro-Level Data Analysis
1. Cumulative Geographic Burden (n=148)
The distribution of 148 laboratory-confirmed cases reveals a persistent, low-intensity spread that spans across multiple regions. While large urban centers initially dominated the statistics, the recent case in Salima demonstrates that the virus is successfully exploiting mobility corridors. This geographic burden analysis suggests that surveillance cannot be localized; rather, a nationwide “blanket” surveillance approach is necessary to capture infections in districts that may not have high healthcare-seeking behavior but are nonetheless at risk.
Strategically, this data indicates that the 148 cases represent only the “tip of the iceberg.” For every confirmed case, there is a statistical likelihood of sub-clinical or asymptomatic cases within the community. Public health efforts are therefore prioritizing districts with high population density and frequent transit, using this geographic data to allocate diagnostic kits and protective equipment where they are most likely to encounter the next “sentinel” case.
2. National Epicurve & Temporal Dynamics
The national epicurve illustrates the temporal progression of the outbreak since April 2025. Unlike explosive outbreaks, Mpox in Malawi exhibits a “smoldering” pattern, with sporadic cases occurring regularly over several months. The confirmation of Case 148 in late January 2026 confirms that the transmission cycle has not been broken. This trend analysis is vital for predicting seasonal peaks and ensuring that the healthcare system is prepared for sustained engagement rather than a short-term emergency response.
Mathematically, the presence of the Salima case on the tail end of this curve suggests that the virus remains endemic in certain reservoirs. The epicurve analysis informs our Risk Communication and Community Engagement (RCCE) strategies—shifting from high-volume general awareness to targeted, behavior-change messaging in districts showing new activity. Constant vigilance is required to ensure that this smoldering trend does not ignite into a large-scale resurgence as environmental and social conditions fluctuate.
Preventative Clinical Directives
Public Safety Protocols
- Zero Contact: Avoid all skin-to-skin contact with individuals presenting unexplained rashes or blisters.
- Sanitization: Mandatory hand hygiene with soap and water or alcohol-based sanitizers in all public transit hubs.
- Immediate Reporting: Any individual with fever and rash must report to the nearest health facility within 24 hours.
Surveillance Mandate
Following the Salima case, PHIM has mandated enhanced surveillance for all district hospitals. Health workers are directed to treat all “Fever + Rash” presentations as suspected Mpox until PCR results prove otherwise. This high-index of suspicion is our primary defense against widespread community transmission.