IDSR Bulletin Epi-Week 43
Editorial Team: Dr. Matthews Kagoli, Mrs. Mtisunge Yelewa, Mr. Austin Zgambo, Mr. Sikhona Chipeta, Mr. James Jere, and Mr. Noel Khunga
Publisher: Moses Nyambalo Phiri
Published on October 30, 2025
Summary of Surveillance (Oct 20-26, 2025)
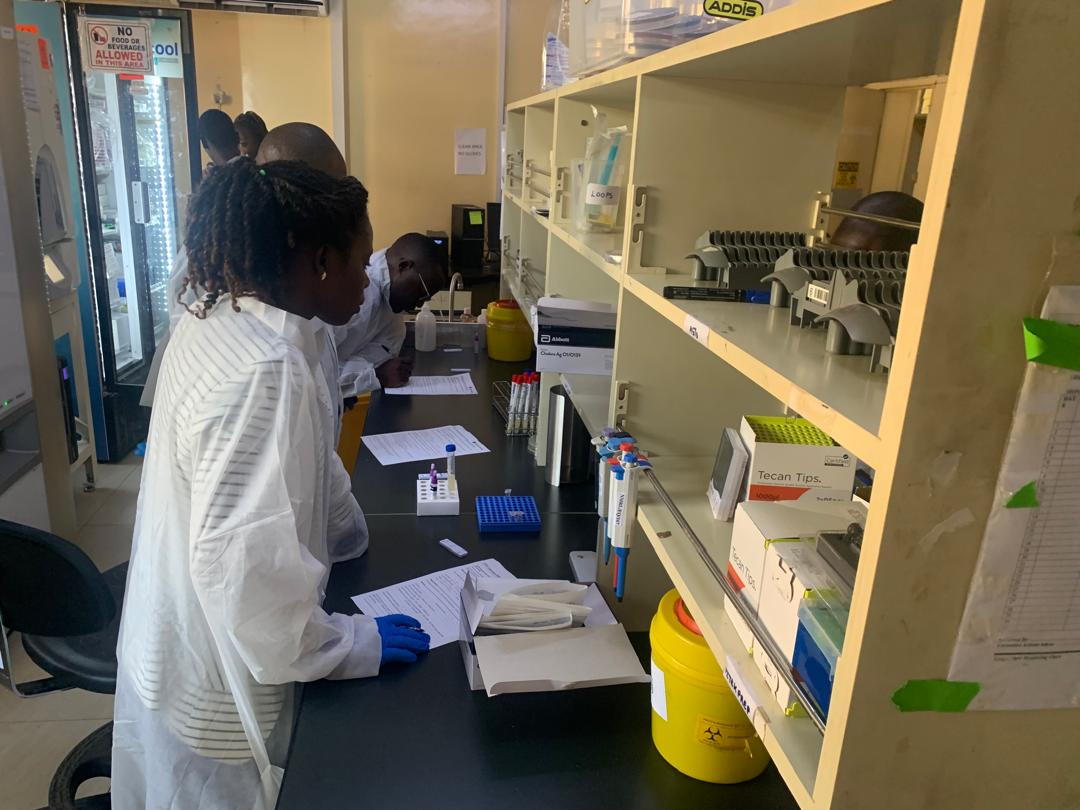
The latest Weekly IDSR Epidemiological Bulletin from the Public Health Institute of Malawi (PHIM) highlights robust surveillance activity for Epi-Week 43. Our Integrated Disease Surveillance and Response (IDSR) system continues to operate effectively, providing critical, timely data to guide the national public health response. This week’s key focus included monitoring a persistent Mpox threat and maintaining high standards for outbreak detection across the country.
Spotlight: Mpox Activity and Event-Based Signals
A significant portion of the week’s effort was dedicated to addressing multiple alerts concerning diseases of public health importance. Event-Based Surveillance (EBS), which captures information on potential threats reported outside routine channels, generated 42 signals requiring immediate investigation by District Rapid Response Teams (DRRTs).
Priority Alert
4
New Confirmed Mpox Cases
Investigation Status
56
Mpox Alerts Reported
High Vigilance
1
Cholera Alert Reported
Other critical alerts managed included Severe Acute Respiratory Infections (SARI) (38 cases, including 4 deaths), Diarrhoea with blood (1,023 cases), Adverse Events Following Immunization (AEFI) (112 cases), and Maternal Deaths (2 deaths). The consistent reporting of these events underscores the importance of maintaining strong vigilance at the community and facility levels.
IDSR Performance Metrics
Performance of the Integrated Disease Surveillance and Response system, tracked via the One Health Surveillance Platform (OHSP), remains robust, though targeted improvements are required.
87.2%
IDSR Completeness
84.9%
IDSR Timeliness
Key Directives and Call to Action
To maintain and enhance the integrity of our surveillance data and response capability, the following action points have been issued to stakeholders across the health system:
- Data Quality & Timeliness: Health facility focal persons and data clerks must improve the timely verification and validation of data entered into the OHSP. Specific districts (Kamuzu Central Hospital, Dowa DHO, Mulanje DHO) are urged to improve reporting timeliness.
- EBS Improvement: All districts must strengthen Event-Based Surveillance (EBS) signal detection and reporting.
- Immediate Response: District Rapid Response Teams (DRRTs) are mandated to conduct risk assessments for all verified signals (events) without delay.
- Measles Immunity: The Expanded Programme on Immunisation (EPI) must strengthen routine immunization coverage and outreach strategies to enhance population immunity and reduce the incidence of measles and other vaccine-preventable diseases.
- Digital Health: Collaboration with the Digital Health team is ongoing to address the issue of server downtime, which negatively impacts reporting timeliness.
The Public Health Institute of Malawi remains committed to transparent and effective disease surveillance. We acknowledge the commendable efforts of all districts and health facilities whose dedication is vital to protecting the health of the nation. For more details, stakeholders are encouraged to refer to the full IDSR Bulletin (Volume 4, Issue 43 of 2025).
Read the Official Bulletin →